- Introduction
- Symptoms
- Causes
- Diagnosis
- Treatment
- Disease Prevention
Introduction
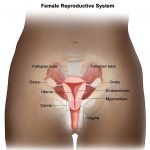
Cervical cancer is the second leading cause of cancer in women under 35, after breast cancer.
Cervical cancer can take years to develop. Before cancer develops, cells in the cervix may show changes known as cervical intraepithelial neoplasia (CIN). These changes can also be referred to as dyskaryosis or carrying precancerous cells.
However, although CIN can develop into cervical cancer if left untreated, the vast majority of women with CIN do not develop the disease.
Some forms of the disease are becoming more and more common. Cervical cancer can be prevented because it can be detected at an early stage through screening programs.
Symptoms
Cervical cancer usually does not cause symptoms unless it has spread to other parts of the body. It may not cause any symptoms unless it has reached an advanced stage. This is why systematic screening programs (cervical smear tests) are so important.
Sometimes there is bleeding between periods or after intercourse, discomfort during intercourse and discharge of foul-smelling fluid from the vagina, but there are no striking early symptoms. Pain and general discomfort are rare until it is in its late stages.
Causes
Although cervical cancer is more common in women with genital warts, these warts are not the cause of the changes in the cervix. Other factors that seem to be related to the disease are the number of sexual partners (a higher number increases the risk), a sexual partner with genital warts, excessive smoking, early pregnancy or three or more pregnancies.
Two viruses are thought to be directly linked to the disease: human papillomavirus (HPV) and herpes simplex (genital herpes) virus.
Diagnosis
Cervical screening diagnoses abnormalities of the cervix that can develop into cancer if left untreated.
Diagnosis is done through the following:
- Physical examination under anesthesia. This usually includes a biopsy of the protective lining of the uterus.
- Colposcopy – an examination using a small light and a microscope.
- Biopsy – taking a sample of cervical tissue for analysis.
- Cone biopsy – a larger area of tissue sample. If small (microinvasive), the abnormal area can be removed in this way or used for diagnostic purposes.
A pathologist’s report will be prepared based on the test results.
If cervical cancer is diagnosed, further tests will be carried out, including
- Blood tests
- X-ray beam
- Pelvic area ultrasound
- Computed tomography scan (CT scan)
- Magnetic resonance imaging (MRI scan)
Treatment
The success of treatment depends on the rate of spread at the time of diagnosis. Early cervical cancer that is confined to the cervix gives a very good outlook with a success rate of more than 85%. If the cancer has spread to the vagina, surrounding tissues and pelvic area or elsewhere, the outlook is more unfavorable.
Surgery, radiotherapy and chemotherapy are all used to treat established cervical cancer, sometimes all together. Radiotherapy usually involves placing tightly closed canisters containing radioactive cesium or radium into the vagina and uterine cavity.
Disease Prevention
Screening with a cervical smear test (pap test) can detect the precancerous stage of the disease. Most women should have this test every three to five years, but those who are particularly at risk should have it at least every year. Your doctor will advise you on how often you should have a smear test.
= = The contents of this page are for informational purposes only. Always consult your doctor for diagnosis and treatment.= =